Jul 22, 2022 | Uncategorized
Download as PDF
If you or someone you love lives with bipolar disorder, please take the time to read this article. Also be aware that abrupt discontinuation of medication carries serious risk of relapse. Always consult with a doctor before changing your medication.
Why Generic NTI’s Are Unsafe
A Statement of Facts
Introduction
In the World War II historical drama The Imitation Game, Alan Turing and his team manage to decode a radio transmission warning of an imminent Nazi attack to an ocean freighter. They are anguished, knowing that if the British Navy acts upon their warning, it will tip off the Nazis to the existence of this newly developed ENIGMA decoder machine, potentially resulting in far greater loss of life. The information they have gleaned is too dangerous to be used.
Public discussion of the issues with the safety of generic Lithium raises a similar paradox.
For many patients, there is no good alternative treatment available. Reports that the drug was unsafe would cause many patients to abruptly stop taking the drug, putting them at high risk of withdrawal symptoms. While the issues surrounding the safety of generic Lithium are well-known to clinicians and pharmacists, they may be hesitant to raise the alarm in the media because the consequences to patients from abrupt withdrawal may be even worse.
Yet over the border in Canada, a safe and effective prescription may be obtained for approximately $30 US per month. Closer to home, new laser measurement techniques make routine quality screening possible and affordable for every prescription filled–if there were only a market incentive to make this technology widely available.
All Lithium prescriptions in the United States have been generic since Eskalith (formerly manufactured by GlaxoSmithKline) was discontinued in 2008. The drug, still widely used to treat bipolar disorder, is on the World Health Organization’s list of essential medicines and is the 205th most commonly prescribed drug in the US. Over 2.6 million Lithium prescriptions were filled in the United States in 2019.
The problems with the generic drug supply in the US have been well documented in such books as Bottle of Lies: The Inside Story of the Generic Drug Boom, by Katherine Eban. This New York Times editorial does an excellent job of summarizing Eban’s main arguments.
However, the pitfalls of generic Lithium are even more severe, due to the drug’s narrow therapeutic range.
For a Narrow Therapeutic Index (NTI) drug like Lithium, the dosage required to be effective is very close to the amount that is toxic and potentially fatal. This poses a problem for the FDA’s current drug regime, known as bioequivalence, because the strength of generic medication in each dose is permitted to vary between 80% and 125% of the prescribed dosage.
This means that an individual who is prescribed a safe-but-high dose of Lithium (for instance, 1500 mg daily) might in fact, on any given refill, find themselves taking a daily dose of 1875 mg… a dose high enough to cause symptoms of Lithium toxicity and organ damage.
End “Lithium Roulette.”
Taking daily medication should never be a gamble. But that’s exactly what people experience when taking Lithium, one of the oldest and most trusted medications for treating mood disorders. Lithium is only available in generic form in the US, and FDA regulations allow the actual dosage of generics per pill to vary between 80 and 125% of the prescribed dosage. This “one-size-fits-all” approach, known as bioequivalence, ignores the fact that certain medications, such as Lithium, require precision dosage. Dosage fluctuations produce toxicity at the high end of the range, and trigger withdrawal symptoms and relapses at the low end. As far back as 2010, the FDA voted to tighten the allowable dosage standard for Lithium and other Narrow Therapeutic Index (NTI) drugs, but these recommendations were never enacted. It is time to hold healthcare providers and generic drug manufacturers accountable.
Abstract
This document describes an issue with drug safety which has played a role in more than 20,000 deaths in the United States since 2008. If not addressed, it will unquestionably result in many more deaths. Because these are deaths by suicide, they tear apart families and bring anguish to loved ones like nothing else
- The vast majority of these deaths are preventable.
- Improving the quality, safety, and dose consistency of generic Lithium is inexpensive and attainable with current technology.
- Bureaucratic apathy and medical negligence are to blame for the current crisis.
Once prescribers, psychiatric associations, and generic drug manufacturers are held accountable, those affected may be able to receive compensation and rebuild their lives. Most important of all, an essential and lifesaving medication may again be made safely available in our country.
Witnesses
I am aware of three doctors, all MDs with years of experience in the practice of psychiatry, who may be contacted to provide testimony that generic Lithium is unsafe.
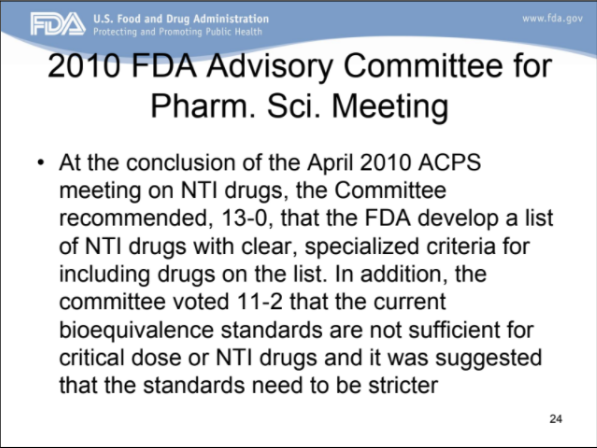
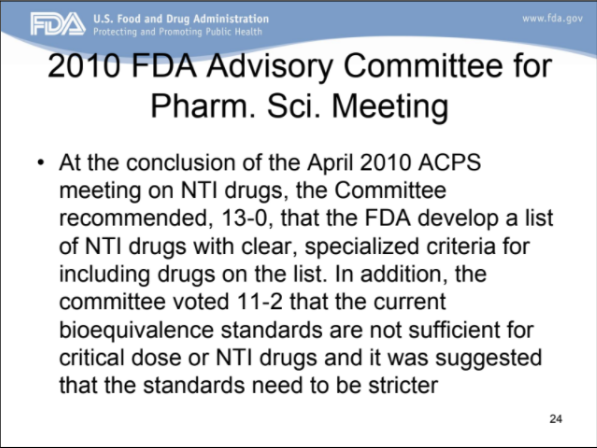
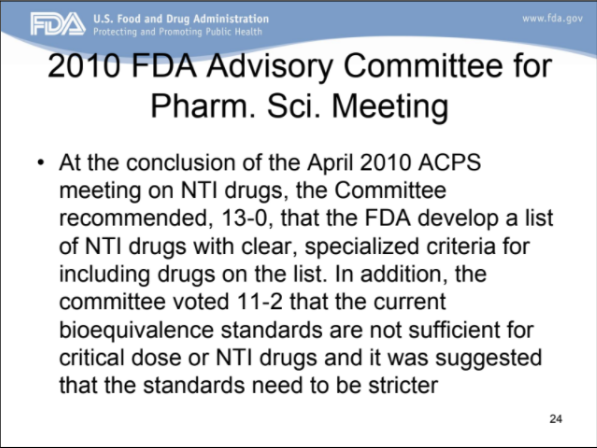
The FDA recommended stricter bioequivalence standards for Lithium as early as 2010.
Source: https://fda.gov “Quality and Bioequivalence Standards for Narrow Therapeutic Index Drugs,” p. 24. An archived PDF file for this presentation may be viewed and downloaded here.
Midway through the first term of the Obama administration, the FDA announced its intention to adopt stricter standards for generic Lithium and other drugs with similarly narrow therapeutic ranges. In 2010, an FDA committee voted 11-2 that the current bioequivalence standards were not sufficient for Narrow Therapeutic Index drugs [including Lithium] and it was suggested that the standards need to be stricter.
Sadly, we find no evidence or public record showing that these recommendations were ever enacted. Faced with little public awareness of the issue, lack of professional engagement and interest from doctors, their professional associations, and other potential “watchdogs,” it would appear that the FDA never followed through with their stated intention. Under the Trump administration, public discussion of changes to bioequivalence standards ceased altogether.
Here is a firsthand account of what this type of Lithium poisoning looks like:
“…two years ago, my nurse practitioner (psych) discontinued my Depakote and started me on Lithium due to unrelenting depression. I was okay for three days on the 300 mg twice a day, but when I increased it to 600 mg twice a day, according to her instructions, I became very ill, very suddenly.
I was so ill I didn’t recognize it myself and never attributed it to my change in medication. I was totally confused, couldn’t walk in a straight line, and was vomiting several times a day. I know now the green haze that I saw is due to Lithium toxicity but thought it odd at the time.
Needless to say, I had to go to the ER and they kept me in. I had Lithium poisoning and had five times the level in my blood. Nearly died. I was very sick indeed for two days in hospital, then released home with two new diagnoses: hypertension and kidney disease which are now being treated with medication, but not welcome diagnoses at all.”
– Sally Alter, on Quora.com
The author of the post does not realize it, but the symptoms she describes are entirely consistent with being prescribed generic Lithium at the high end of the current dosage range allowed by the FDA. It is especially telling that she was able to tolerate Lithium at an earlier period in her life and encountered no problems.
Prescribers who know of these risks and do not inform their patients, insist on the necessary blood tests, or advocate for stricter standards are in violation of their Hippocratic Oath.
Lithium toxicity, while the most dramatic byproduct of the current negligence in bioequivalence standards, is only the tip of the iceberg.
Bipolar disorder affects about 5.7 million adults in the United States, and the fatality rate is staggering–as high as 20 percent. Nearly 12,000 lives are lost to bipolar suicide each year. Lithium remains the first-line treatment for many individuals experiencing bipolar disorder. We see evidence of its declining effectiveness in the population at large. Success rates of 70 to 85% were once expected with lithium for the acute phase treatment of mania, however, lithium response rates of only 40 to 50% are now more common.
Using the most conservative assumptions possible, we should assume that over the past 14 years, generic Lithium was a factor in at least 20,000 of these deaths. This figure is derived from 12,000 bipolar suicide deaths per year x 12 years x reported Lithium usage rate of 14.3% = 20,592 deaths. For data on rates of Lithium usage for patients in the United States from 1996-2015, see https://pubmed.ncbi.nlm.nih.gov/32739706/
This estimate is low, since it does not include those people who discontinued generic Lithium after experiencing toxicity or relapse.
Why would generic Lithium be a culprit?
Because variation in dose strength leads to relapse.
Relapses lead to acute mood swings: bouts of psychotic mania and extreme depression that may themselves lead to suicidal actions, or to the words and actions that destroy relationships, marriages, and careers. Even if the first relapse does not kill somebody, it may leave them dangerously isolated and vulnerable. The effect is to decrease an individual’s belief in the effectiveness of medication and increase stigma in the population at large.
“There is no cure for bipolar illness” is one of the most harmful and misleading statements ever coined. For many individuals, including myself, name-brand Lithium with precise dosage was effectively a cure. Now it can only be obtained by venturing outside the United States.
Let’s go back to our hypothetical individual who is prescribed 1500 mg daily of Lithium. Data suggests that the risk of symptoms from abrupt Lithium withdrawal actually exceeds the risk from the untreated disorder. Dose variations in generic Lithium means someone could go from 1875 mg to 1200 mg in dosage over a single refill–enough to cause withdrawal symptoms.
How often does this happen? Remember that Lithium is a maintenance drug. Even if a significant fluctuation in dosage happens with only one drug refill out of 10, if you are bipolar and taking generic Lithium, the odds are that this “yo yo effect” will happen to you at least once every year. If you have a relapse, you will likely wonder what you did wrong and blame yourself, never realizing the role played by drug manufacturers and clinicians who knowingly allowed an unsafe product to remain available to consumers.
My Story
In 2018, I was about to embark on the seed round of fundraising for my social media and cryptocurrency startup. We had a great product and a terrific founding team. Everyone involved was optimistic about our chances. One of our early investors asked me to apply for life insurance. I was surprised to learn I did not qualify, due to the high death rate associated with my diagnosis. I was healthy and under a doctor’s care. It made no difference.
Being unable to obtain what it is known as “Key Man” insurance meant that my hopes of launching a venture-backed tech startup were dashed. I turned my passion and energy towards wellness coaching instead, hoping that I could make a difference and model a successful outcome for individuals struggling with mood disorders.
Operating with almost no name recognition or word of mouth, I quickly connected with a large pool of coaching clients. The experience was rewarding, but it also made me aware of the shortcomings of our mental health care system–in particular, the issues surrounding generic mood stabilizers.
My frustration with the treatment options available to persons with mood disorders led me to eventually close my practice. I did not wish to profit from a system that was so seriously broken. I was committed to working with doctors and licensed clinicians, and would only see clients who already had a doctor and/or therapist. However I did not feel I could be honest about the risks associated with drug therapy without a scalable, accessible solution at hand.
Conclusion
If you are prescribed Lithium, you should expect to have your blood drawn several times each year in order to determine whether your Lithium blood level is in the therapeutic range, or whether the serum level is too low or too high. That is what is entailed when prescribing and monitoring a potentially toxic drug with a narrow therapeutic range. The experience is painful and inconvenient, but medically necessary. Dosage fluctuations have transformed this established medical procedure into an empty ritual.
This is not an issue of side effects or isolated incidents of poor quality control. This is an issue of systematic negligence which has rendered one of the most important and trusted treatments for a life threatening disease to lose its effectiveness, and in some cases be worse than no treatment at all. Because of the risks from abrupt Lithium withdrawal, those most directly impacted cannot even safely cease taking the medication. We are looking at a situation where a serious and well-known safety issue was ignored for over a dozen years. Care providers, drug manufacturers, and professional associations who should have been motivated to act on behalf of patient safety instead did next to nothing. Apathy and inaction led to death.
Many people have experienced Lithium toxicity and preventable manic or depressive episodes due to negligent bioequivalence standards, but the most tragic harm rests with the individuals who have lost their lives, and with their families. Potentially, the pool of people harmed includes anyone with a family member who took generic Lithium and then had one or more episodes before ultimately committing suicide. These stories number in the tens of thousands. Practices, prescribers, professional associations, and generic drug manufacturers all bear responsibility.
Stigma is a major factor that keeps successful, high-functioning bipolar people from organizing for better care, more research, and treatments that actually work! We remain closeted and are busy living our lives until the moment when illness strikes us down. Earlier in this document, I alluded to an anecdote from Alan Turing’s life. Readers may be aware that Turing died by suicide, driven largely by homophobia and repression from the British government. Unless you have actually lived through prejudice, it is very difficult to comprehend the experience of being hated and shunned for something you cannot control. This was certainly the hardest lesson for me to learn as a wellness coach. I had never before had to face hatred head-on.
This barrier of ableism may be the greatest challenge to restoring justice and safe standards for an irreplaceable medication. I believe it is surmountable. Lives are at stake.
If you or someone you know is in crisis or experiencing suicidal thoughts, please call 988 or contact one of the many Crisis Resources listed on our site.
Download as PDF

May 14, 2020 | Front Page, Health
First Aid for Attempted Suicide
Article by Sarah Gehrke, MSN, RN. Reprinted with permission from https://pacificmedicalacls.com.
Suicide touches all ages and incomes; all racial, ethnic, and religious groups; and in all parts of the country. It is a leading cause of death in the US.
As self-inflicted injuries increase so does the need to prepare for encountering someone who has attempted suicide. As a first-aid provider, you have a vital role in addressing immediate medical needs. You can also provide clarity and support to the victim and other people at the scene.
In 2017, guns were the most common method of death by suicide, accounting for a little more than half of all suicide deaths. The next most common methods were suffocation at 27.72 percent, and poisoning at 13.89 percent.
The following first-aid recommendations are for each of the most common methods of attempted suicide. Each case is unique, and it is essential to tailor your care and support to that person’s needs.
Above all ensure the safety of everyone present and address any serious medical needs first.

© Staff Sgt. Natasha Stannard / Joint Base Langley-Eustis / CC-BY-SA-3.0
First Aid for Gunshot Wound
A self-inflicted gunshot wound (SIGW)—or any gunshot wound—to the head is correlated with severe disability and a high mortality rate. There is a greater chance of death caused by SIGWs compared to victims injured by gunshot wounds that are delivered in an assault or by accident.
- Head trauma from a gunshot wound is fatal in about 90 percent of cases, with many victims dying prior to arriving at the hospital.
- About 50 percent of the victims that survive the initial trauma die in the emergency department.
- Head trauma from a gunshot wound is the cause of approximately 35 percent of deaths attributed to traumatic brain injury.
Although the head is the most commonly injured body region during a suicide attempt, the following is a general guideline for how to approach a gunshot wound on any area of the body.
- Ensure your safety. Ensure the scene is safe and immediately call or have someone else call 9-1-1 or emergency medical services.
- Locate the source of the bleeding. Attempt to open or remove the clothing over the wound so you can see it—this will allow you to see injuries that may have been covered or hidden.
- Stop the bleeding. Pressure to stop the bleeding is the most critical intervention. If the victim has blood that is coming out of a hole, put steady pressure on it with both hands by pushing down as hard as you can.
- Use a dressing (towels, shirts, gauze, etc.). Dressings will help seal the wound and aid in clotting.
- Elevate the extremity. If the gunshot wound is above the waist do not elevate the legs to treat for shock (unless the injury is in the arm). Gunshot wounds to the chest and abdomen will bleed more rapidly if the legs are elevated, thus making it more difficult for the individual to breathe.
- If you can, use a tourniquet. Tourniquets will only work on arm and leg injuries. Using them correctly takes practice, and they should only be used if the bleeding cannot be stopped when direct pressure and elevation are applied immediately and simultaneously or if there is a reason why direct pressure cannot be maintained.
- Gunshot wounds to the chest may be sealed with a type of plastic to keep air from being sucked into the wound—this can help prevent a collapsed lung. Remove the seal if shortness of breath worsens after sealing the wound.
- Chest compressions in a cardiac arrest caused by hemorrhagic shock from severe blood loss may worsen the situation.
First Aid for Hanging or Suffocation
Self-administered and assisted suicides by asphyxiation—the process of being deprived of oxygen resulting in unconsciousness or death—can be done by several methods. The use of a plastic bag, or suicide bag, is often in conjunction with a flow of an inert gas like nitrogen or helium.
Suicides using a plastic bag with helium were first recorded in the 90s. Since the 2000s, guides on how to use this method have spread on the internet, in print, and on video; and the frequency of suicides by this technique has increased.
Asphyxiation is also present in hanging and strangling. Both hanging and strangling can obstruct blood flow to and from the brain as well as block air flow to and from the lungs.
How to Recognize Suffocation
- A constricting article is around the neck
- Marks around the victim’s neck where a constriction was removed
- Impaired consciousness or unconscious
- Grey-blue skin (cyanosis)
- Uneven breathing
- Prominent veins and congestion of the face
- Petechiae – tiny red spots on the face or the whites of the eyes
What to Do in the Case of Suffocation
- Make sure the scene is safe, and immediately remove any constriction from around the victim’s neck; support the body if it is still hanging.
- Call or have someone else call 9-1-1 or emergency services.
- Lay the victim on the floor. In the case of spinal injury, don’t move the victim unnecessarily.
- Check for breathing and pulse; If not breathing begin CPR.
- If breathing, place in the recovery position and monitor until emergency responders arrive.
- Don’t interfere with or destroy any material, such as a knotted rope, that police may need as evidence.
First Aid for Overdose or Poisoning
Poisoning is due to swallowing, inhaling, touching, or injecting various chemicals, drugs, gases, or venoms. Both suicide and unintentional drug overdoses kill adults at twice the rate today as they did two decades ago, and opioids are a key contributor to this rise. The following focuses on the use of drugs as a means of attempting suicide.
When a drug overdose is suspected, you may not know what drug the person was taking. Often, an overdose victim will either be unconscious or not fully conscious of their surroundings. Because of this, it is imperative to recognize the general signs of a drug overdose and what to do for first aid in the majority of situations.
How to Recognize an Overdose
- Unusual sleepiness or unresponsiveness
- Confusion, disorientation, or hallucination
- Slow, shallow, irregular, or absent breathing
- Bradycardia (slow heartbeat) or hypotension (low blood pressure)
- Cold and clammy skin
- Constricted pupils (small or pinpoint pupils)
- Cyanotic (nails and lips are blue)
- Mood changes, including aggression, agitation, anxiety, or depression
- Abdominal pain or vomiting
- Loss of coordination or motor control
Do’s for Drug Overdoses
- Make sure the scene is safe, and check alertness. Comfort them if they are awake. If they are unconscious, turn them on their side to prevent aspiration (choking on their vomit).
- Call 9-1-1 or emergency medical services. Call, or have someone else call, even if the person seems not to be experiencing overdose symptoms; never wait to see if the overdose will wear off. Some effects of an overdose don’t present themselves right away.
- Check for breathing and pulse; If not breathing begin CPR.
- Remove unnecessary clothing if the situation allows. Some drugs cause the patient to quickly overheat.
- Find details to aid with treatment. Knowing what drug was taken, how much, when, and by what method is important. If the victim is not awake, look for containers, needles, syringes, and other items.
Don’ts for Drug Overdoses
- Don’t put the person in the shower. Even if the victim seems okay, a large temperature change could put them in shock.
- Don’t let the person sleep. Someone who overdosed may pass out, and you will not be able to stop them; however, trying to keep them awake makes it easier to monitor their condition.
- Don’t attempt to make them throw up if they took the drugs orally. This can increase the chance of aspiration.
- Don’t wait for the drug to wear off. Call for emergency medical services immediately.
- Don’t try to feed the victim. Some foods can have adverse effects.
- Don’t leave the victim alone. Stay with them, monitor their condition, and provide help as needed.
- Don’t try to reason with or restrain a violent person or put yourself in an unsafe position.
First Aid for Known Opioid Overdose
Examples of opioids include morphine, codeine, oxycodone, oxycodone with acetaminophen, and hydrocodone with acetaminophen. Because opioids affect the part of the brain that controls breathing, too high of opioid levels in the blood can slow breathing down to dangerous levels, which could cause death.
For victims with a suspected or known opioid overdose who have a definite pulse but no normal breathing or only gasping (respiratory arrest) in addition to providing standard care, it is reasonable for trained rescuers—this includes first aid providers, non-healthcare providers, or BLS providers—to administer Narcan® (naloxone) intramuscularly or intranasally to victims with an opioid-associated respiratory emergency.
Victims with no definite pulse may be in cardiac arrest or they may have an undetected slow or weak pulse. These cases should be managed as a cardiac arrest victim.
Standard resuscitation should take priority over the administration of naloxone, with a focus on high-quality CPR. It may be reasonable to administer naloxone—especially when an opioid overdose is suspected—based on the possibility that the victim is in respiratory arrest, not cardiac.
Opioid-Associated Life-Threatening Emergency (Adult) Algorithm
- Assess and activate. Check for unresponsiveness and call for nearby help. Send someone to call 9-1-1 and get AED and naloxone. Observe for breathing versus no breathing or only gasping.
- Begin CPR. If the victim is unresponsive with no breathing or only gasping, begin CPR (CPR technique based on the rescuer’s level of training). If alone, perform CPR for about 2 minutes before leaving to phone 9-1-1 and get naloxone and an AED.
- Administer naloxone. Give naloxone as soon as it is available. 2 mg intranasal or 0.4 mg intramuscular. May repeat after 4 minutes.
- Does the person respond? If yes, stimulate and reassess. Continue to check responsiveness and breathing until advanced help arrives. If the person stops responding, begin CPR and repeat naloxone. If no response, continue CPR and use an AED as soon as it is available. Continue until the person responds or until advanced help arrives.
First Aid for Self-Harm or Self-Cutting
Because self-harm, also known as self-injury or self-cutting, involves physical injury, it can seem like self-harm and suicide are directly related. For example, it is common to think that cutting one’s wrist may be a suicidal gesture indicating that the person wishes to slit their wrists to die.
Self-injury can indicate a number of different things. Many people who practice self-injury may not intend to kill themselves and may even see self-harm as a way of avoiding suicide. It is crucial to note that with the pattern of self-injury occurring over weeks, months, or years, the person may be at risk for suicide.
Here’s what you should do if you a self-harm situation presents to you:
- Make sure the scene is safe, and assess and activate. Assess the victim’s responsiveness. Call or have someone else call 9-1-1 or emergency services.
- Locate and control the bleed. Arterial blood is bright red and spurts or sprays from the wound. If the blood is darker in color and easier to control, it means that the veins have been cut, and the artery was missed.
- Apply direct, firm pressure. Apply a towel or dressing directly to the wound.
- Elevate. Position the wounded limb in a position where it’s above the victim’s heart.
- Occlude or pinch an artery above the injury. If possible apply pressure to an artery to halt the blood supply to that limb. If the bleeding does not stop after direct pressure, a tourniquet may be needed.
- Assuming the bleeding has stopped, continue to assess the victim—circulation, airway, and breathing. Follow the Basic Life Support (BLS) Algorithm.
If You Know Someone in Crisis:
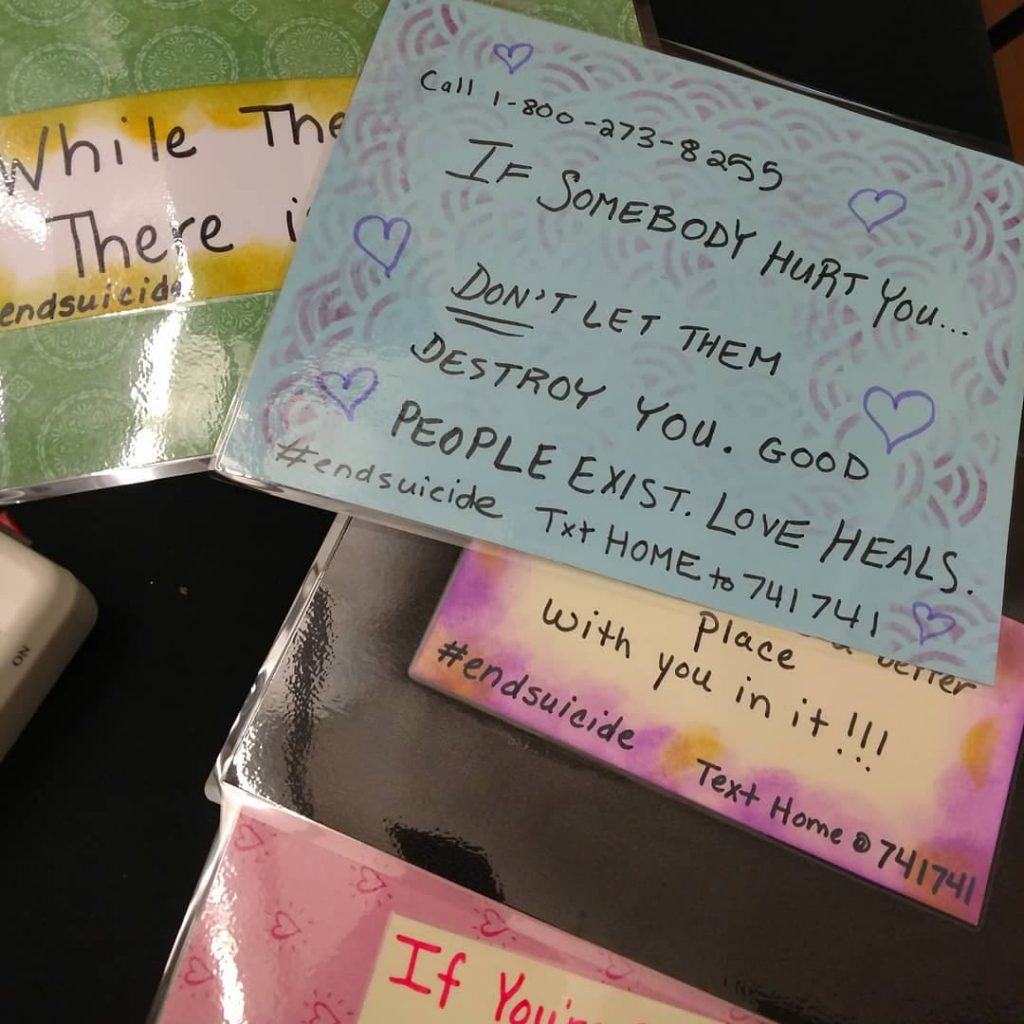
Call the toll-free National Suicide Prevention Lifeline (NSPL) at 1–800–273–TALK (8255), 24 hours a day, 7 days a week. The service is available to everyone. The deaf and hard of hearing can contact the Lifeline via TTY at 1–800–799–4889. All calls are confidential.
Washington State Crime Victim Service Center Hotline: 888.288.9221
Contact social media outlets directly if you are concerned about a friend’s social media updates or dial 911 in an emergency.
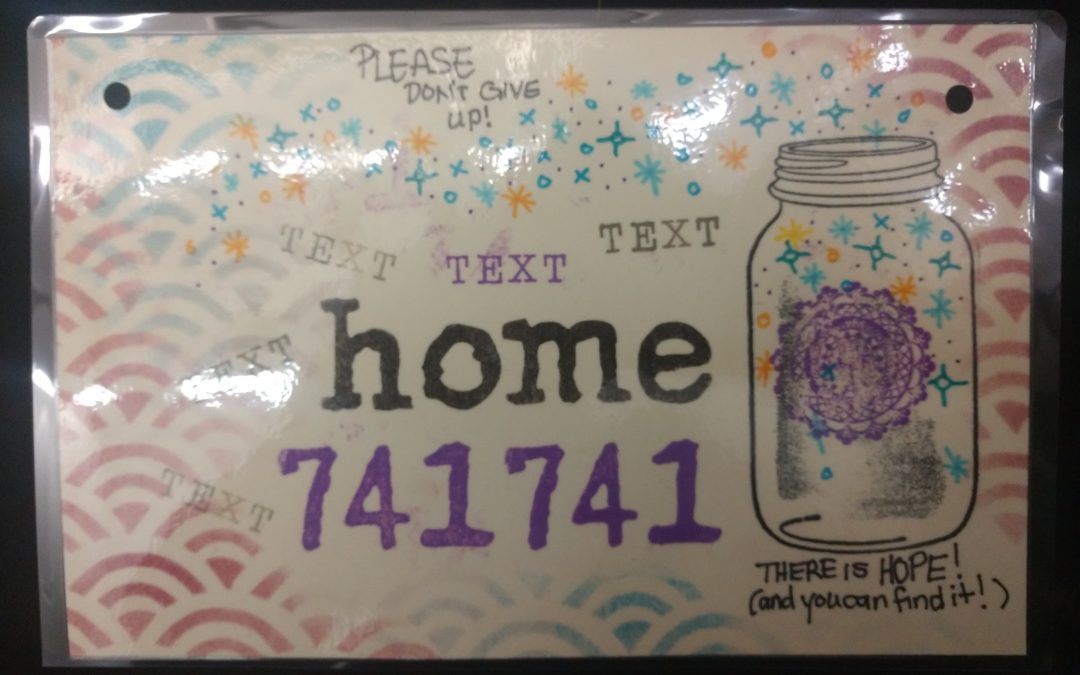
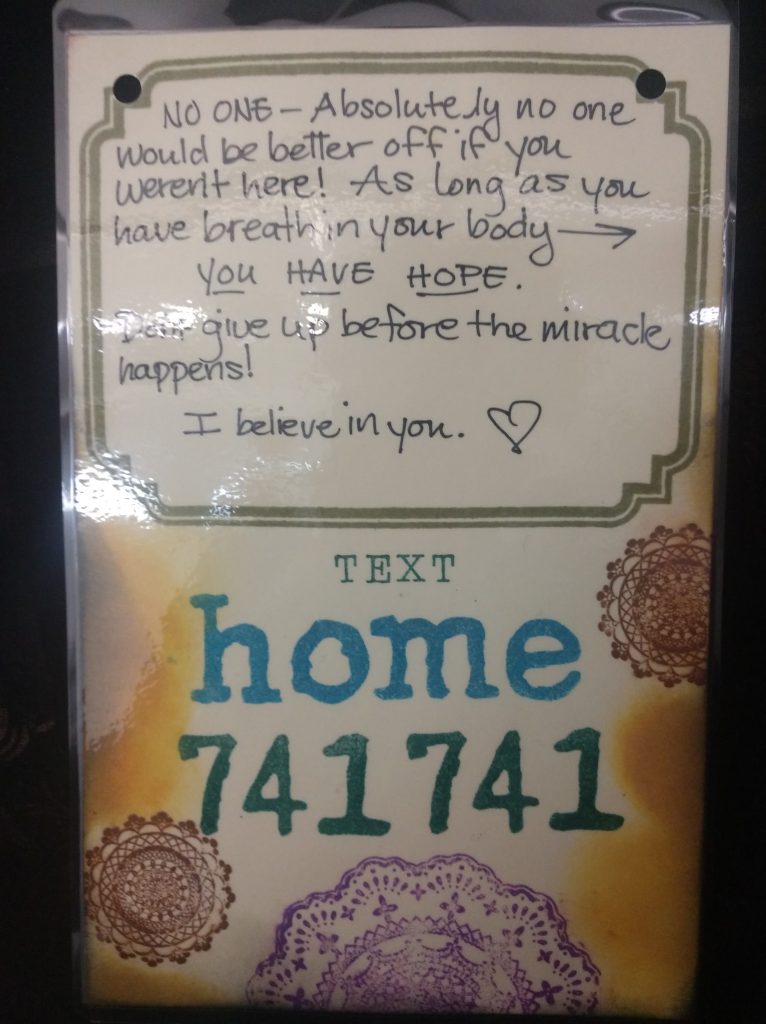
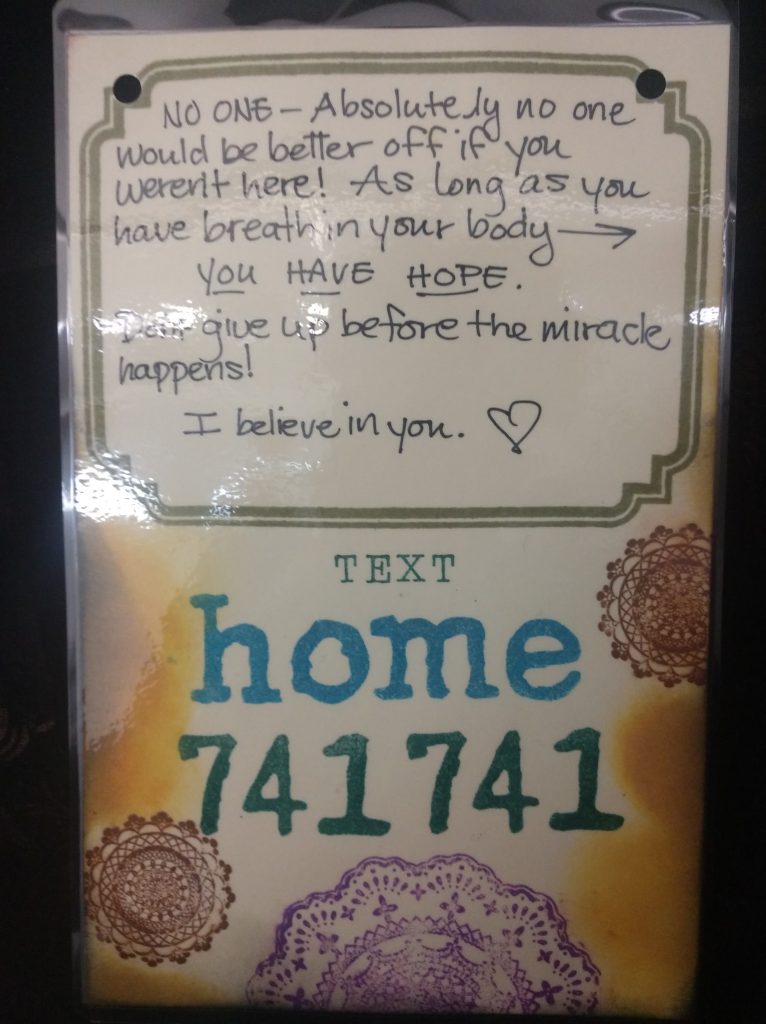
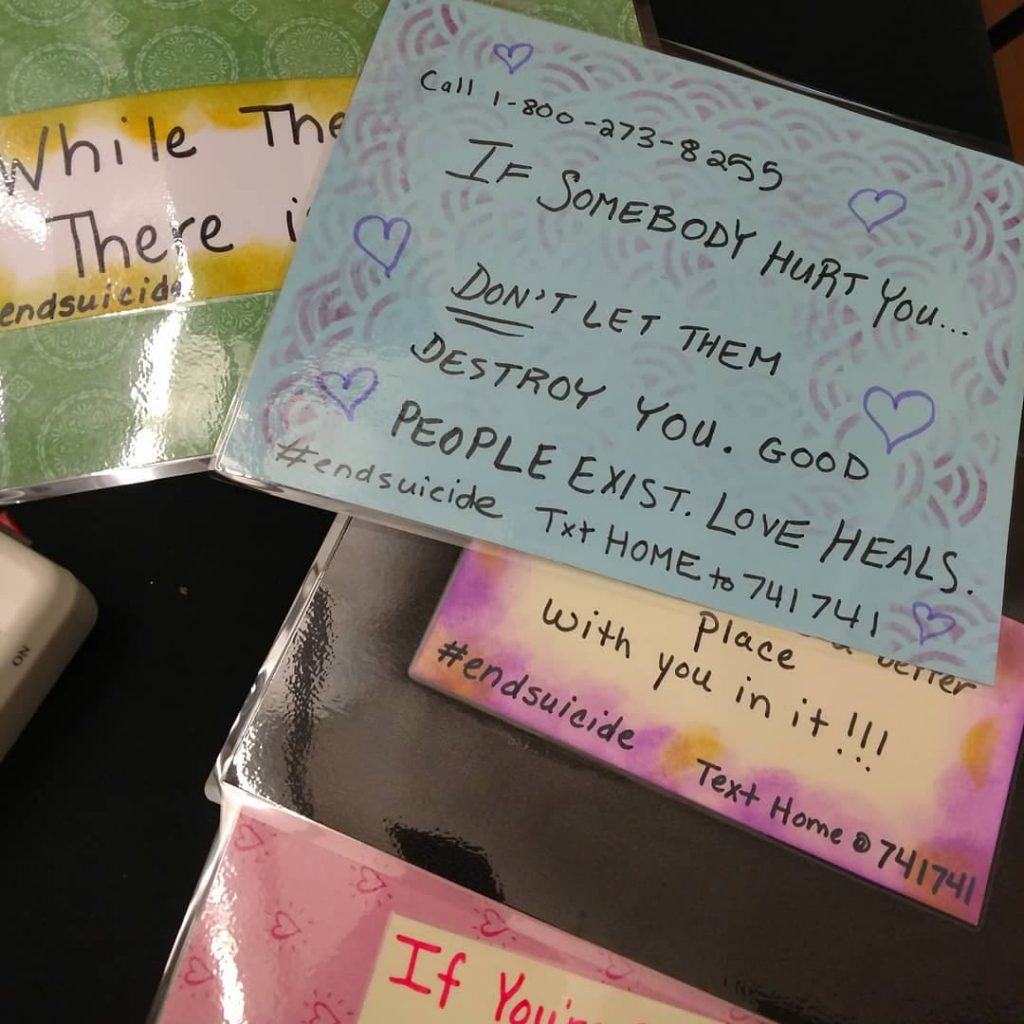
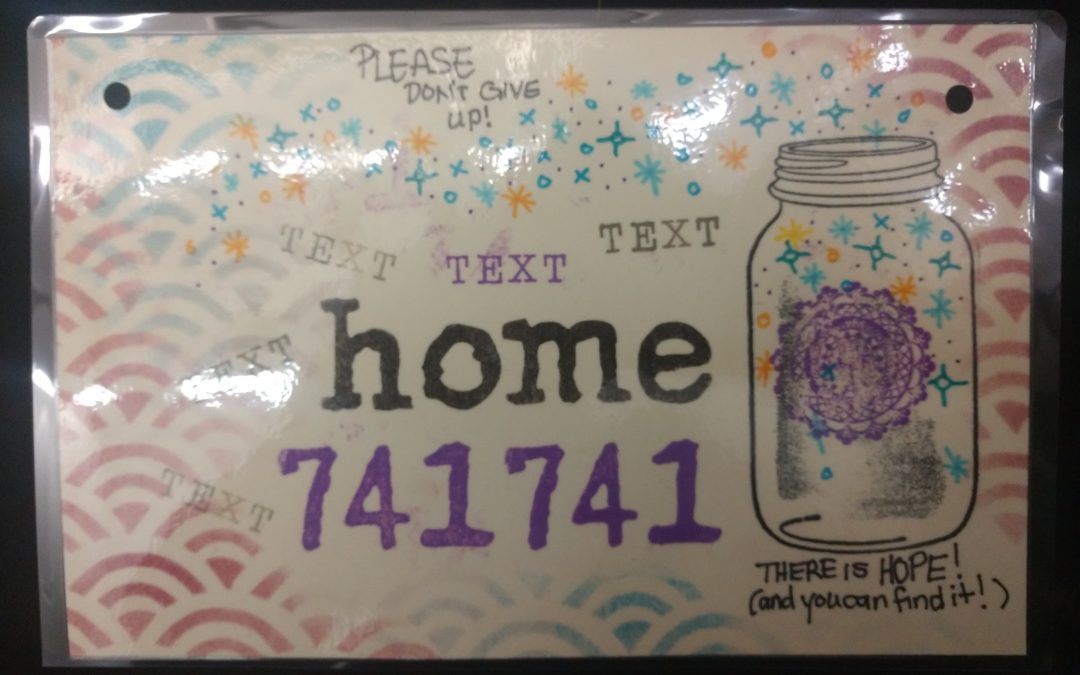
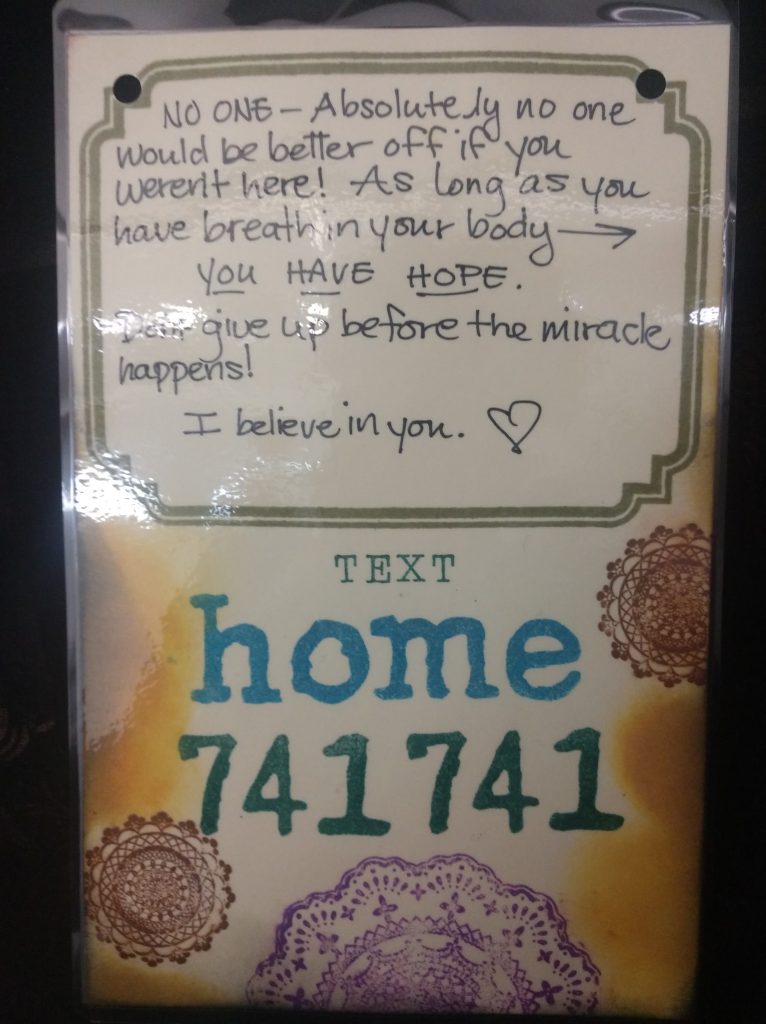
Learn more on the NSPL’s website. The Crisis Text Line is another resource available 24 hours a day, 7 days a week. Text “HOME” to 741741.
Mar 29, 2020 | Front Page, Health, Uncategorized
We’ve put together a list of helpful national and local Portland, OR and Seattle, WA resources for mental health and suicide prevention, updated for COVID-19. Please let us know if any of these links are broken, or if you have new ones to suggest. Thank you, and be well.
Helplines
https://suicidepreventionlifeline.org The National Suicide Prevention Lifeline at 988 (formerly 1-800-273-8255) provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals. Telephone and online chat available.
https://calltosafety.org A Call to Safety advocate can connect you with resources through the crisis line, or you can explore some Portland Metro resources below. Learn more about domestic and sexual violence, stalking, and sex work on our site.
https://oregonyouthline.org For teens, they can call, text, chat and during certain hours can talk to peer support.
https://www.crisistextline.org Crisis Text Line, text HOME to 741741.
http://communitycounselingsolutions.org/warmline A peer-run program of Community Counseling Solutions.
IAPMD.org The International Association for Premenstrual Disorders (IAPMD) is a not-for-profit organization providing education, support, advocacy, and resources for those affected by Premenstrual Dysphoric Disorder (PMDD) and Premenstrual Exacerbation of underlying disorders (PME).
https://www.translifeline.org Peer support, hotline, and resources for the trans community.
https://www.thetrevorproject.org A national 24-hour, toll free confidential suicide hotline for LGBTQ youth.
503-575-3764 – Crisis Line for Racial Equity Support – Answered by BIPOC counselors M-F from 8:30 AM -5:00 PM.
877-226-3111 – Addiction Hotline
1-855-227-3640 – Caregiver Help Desk Hotline
503-300-1633 – Clackamas Senior Loneliness Line
844-228-2962 – Eating Disorder Hotline
877-455-0628 – Self Harm Hotline
888-640-5174 – Depression Hotline
Clackamas County Mental Health Crisis Line (503) 655-8585
Multnomah County Mental Health Crisis Line (503) 988-4888
Washington County Mental Health Crisis Line (503) 291-9111

Seattle Mental Health Crisis Line (866) 427-4747
Community Resources
https://www.nami.org NAMI, the National Alliance on Mental Illness, is the nation’s largest grassroots mental health organization dedicated to building better lives for the millions of Americans affected by mental illness. Oregon NAMI Chapter: https://namior.org/
http://gettrainedtohelp.com – Suicide First Aid. Free trainings in suicide prevention for the general public, youth workers, and more. Includes the ASIST curriculum.
https://grantsforseniors.org – Website to guide seniors and retirees when they need help. Includes categories such as financial help, health care, food, housing, and transportation assistance, as well as help and resources for daily life.
https://www.facebook.com/groups/stjohnssuicideprevention – St. John’s Suicide Prevention Team. A community group helping reduce the incidence of suicides in Portland, Oregon and the St. John’s neighborhood.
https://multco.us/mhas/mental-health-crisis-intervention – Multnomah Crisis Intervention Resources (includes walk-in clinic).
https://www.co.washington.or.us/hawthorn – Walk-in trauma intervention program in Washington County.
http://www.seattlecrisis.org/counseling.html – Counseling and mental health resources for Seattle, WA.
https://www.mentalhealthfirstaid.org – Nationwide organization providing training to help someone who is developing a mental health problem or experiencing a crisis.
https://mesotheliomahub.com/mesothelioma/patient-resources/suicide – Suicide Prevention & Cancer Patients
Substance Abuse
https://www.samhsa.gov/ebp-resource-center/ – Federally funded Evidence Based Practices Resource Center for mental and substance abuse disorders.
https://www.drugrehab.com/guides/suicide-risks/ – A guide to understanding the connection between Substance Abuse & Suicide.
https://www.detoxrehabs.net/ – This site helps you find centers in your home state or out of state. We also provide information for different community needs, such as help for our veterans, LGBTQ+ friendly programs, free or Medicaid accepting treatment, and pet-friendly facilities.
www.AlcoholRehabGuide.org – This guide doesn’t promote any specific clinic or service, but it does provide valuable information to help people understand the effects of alcoholism and the variety of ways to find help.
www.alcoholhelp.com – Browse resources and get connected to treatment that is right for you.
Hashtags
#endsuicide #worldmentalhealthday #suicideawareness
Mar 22, 2020 | Uncategorized
I’ve put together a list of helpful national and local Portland, OR and Seattle, WA resources for mental health and suicide prevention. This list reflects that there is no one-size fits all solution — text or online chat may be a better option for somebody who doesn’t have privacy to talk, and with “warmlines,” people may wish to seek help even if their life is not imminently in danger. Please let me know if any of these links are broken, or if you have new ones to suggest. Thank you, and be well.

Founding Members of the St. John’s Suicide Prevention Team: Elizabeth Gadwa, Laura Bee, and Kristen Gray
Helplines
https://suicidepreventionlifeline.org The National Suicide Prevention Lifeline at 988 (formerly 1-800-273-8255) provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals. Telephone and online chat available.
https://oregonyouthline.org For teens, they can call, text, chat and during certain hours can talk to peer support.
https://www.crisistextline.org Crisis Text Line, text HOME to 741741.
http://communitycounselingsolutions.org/warmline A peer-run program of Community Counseling Solutions.
IAPMD.org. Resources and support geared specifically to individuals living with PMDD (Premenstrual Dysphoric Disorder).
https://www.thinkpacifica.com/anxiety-peer-support-groups Free online support peer support groups for stress, anxiety & depression.
https://www.translifeline.org – Peer support, hotline, and resources for the trans community.
https://www.thetrevorproject.org – A national 24-hour, toll free confidential suicide hotline for LGBTQ youth.
503-575-3764 – Crisis Line for Racial Equity Support – Answered by BIPOC counselors M-F from 8:30 AM -5:00 PM.
877-226-3111 – Addiction Hotline
1-855-227-3640 – Caregiver Help Desk Hotline
503-300-1633 – Clackamas Senior Loneliness Line
844-228-2962 – Eating Disorder Hotline
877-455-0628 – Self Harm Hotline
888-640-5174 – Depression Hotline
Clackamas County Mental Health Crisis Line (503) 655-8585
Multnomah County Mental Health Crisis Line (503) 988-4888
Washington County Mental Health Crisis Line (503) 291-9111

Seattle Mental Health Crisis Line (866) 427-4747
Community Resources
https://www.nami.org NAMI, the National Alliance on Mental Illness, is the nation’s largest grassroots mental health organization dedicated to building better lives for the millions of Americans affected by mental illness. Oregon NAMI Chapter: https://namior.org/
http://gettrainedtohelp.com – Suicide First Aid. Free trainings in suicide prevention for the general public, youth workers, and more. Includes the ASIST curriculum.
https://www.facebook.com/groups/stjohnssuicideprevention – St. John’s Suicide Prevention Team. A community group helping reduce the incidence of suicides in Portland, Oregon and the St. John’s neighborhood.
https://multco.us/mhas/mental-health-crisis-intervention – Multnomah Crisis Intervention Resources (includes walk-in clinic).
https://www.co.washington.or.us/hawthorn – Walk-in trauma intervention program in Washington County.
http://www.seattlecrisis.org/counseling.html – Counseling and mental health resources for Seattle, WA.
https://www.mentalhealthfirstaid.org – Nationwide organization providing training to help someone who is developing a mental health problem or experiencing a crisis.
https://mesotheliomahub.com/mesothelioma/patient-resources/suicide – Suicide Prevention & Cancer Patients
Substance Abuse
https://www.samhsa.gov/ebp-resource-center/ – Federally funded Evidence Based Practices Resource Center for mental and substance abuse disorders.
https://www.drugrehab.com/guides/suicide-risks/ – A guide to understanding the connection between Substance Abuse & Suicide.
www.AlcoholRehabGuide.org – This guide doesn’t promote any specific clinic or service, but it does provide valuable information to help people understand the effects of alcoholism and the variety of ways to find help.
Hashtags
#endsuicide #worldmentalhealthday #suicideawareness

Nov 21, 2018 | Front Page, Health
Laura and I are humbled and thrilled with all the media coverage received for our small effort to put up notes of encouragement on the St. John’s Bridge. Read or watch the story by Portland’s Fox 12 here.
But this is really only the beginning. Would you like to take two hours out of your busy schedule and learn how to save a life? We are please to announce a free training available in our community. The two-hour “Suicide First Aid” class, offered through http://gettrainedtohelp.com, a tri-county initiative, is for lay people. No special background is required. It teaches essential skills for responding if somebody you know or love has reached out and appears to be at risk. The one-time session will be held in the evening, from 6-8 PM on Tuesday, January 15. 2019, at Vision 8 Studios at Cathedral Park Place. Training is open to all residents of Portland, OR and the surrounding area; however St. John’s residents have priority. The training is for everyone aged 18 and over.
If you are interested, sign up here.
Please click here for a comprehensive guide to suicide hotlines and other community resources in the area.